Health information: sourcing patterns and quality improvement prior to surgery
Introduction
Twelve point nine million Australians have home internet subscription and almost double this (21.3 million) have access to the internet via mobile handsets (1). The ubiquity of the internet and its technologies has had an effect on the availability of health information and ultimately health choices. There are internet websites and mobile applications that allow patients to self-diagnose and manage their symptoms, though most have not been independently assessed or validated. In the age of patient-centred decision making, healthcare providers must consider the information available to patients through the World Wide Web and its influence. Patients seek information on the internet to reinforce or provide reassurance about the advice given to them by their healthcare provider (2). It is an important tool used by parents to help them make decisions on behalf of their child (3). Terms such as ‘Dr. Google’ touch on the importance of the internet in discussions on individual healthcare decisions and highlight its dangers. A recent literature review found that most information caregivers accessed through the internet was not scientific and of variable value, and calls on healthcare providers to guide and provide them with quality information (3).
The aim of our study was to understand how our patient’s caregivers accessed health care information and what we could do to make them feel better informed. We wanted to look at their opinions on information given to them by their doctor, and how the internet was used to supplement their understanding. In quantifying and comparing the value and use of these two forms of information, we hoped to identify how to improve the information we provide to them in the future and to allot resources towards this appropriately. This should be translatable to other surgical specialities. Changing our clinical behaviours in direct response to patient feedback will improve the quality of the service we provide.
Method
Ethics approval was obtained from the Sydney Children’s Hospitals Network Human Research Ethics Committee. A paper based questionnaire was given to parents of children having an Otolaryngology procedure at a tertiary children’s hospital on the day of surgery. The questionnaire was handed out to the child’s attending guardian by administration staff at the time of checking in to the Day Surgery Unit. A written explanation of the survey, its background and goals were included at the beginning of the document to guide them through completing it. It was left to the guardian’s discretion to complete and return the questionnaire over the course of that day without direct interaction regarding it from the clinical or research team. Recruitment was consecutive from December 2014 to February 2016 in order to ensure at least 100 surveys were received for data analysis.
The questionnaire was four pages long and divided by five headings: “General Data Questions”, “Questions About Booking Your Child’s Operation”, “Questions About the Information You Were Given”, “Questions About Sourcing More Information”, “Questions About Improving the Information Given to Caregivers in the Future”. Data was collected on patient and respondent demographics, the type of procedure they were having on that day and the pre-procedure surgical consultation. They were asked to rank the seniority of the person recommending surgery. We asked respondents to rate on a scale of 1 to 10, their perception and understanding of the information given at the pre-operative consultation. We asked them how and what supplementary sources of information they sought. This data was collected in the form of tick box selection from a list, where multiple responses were possible. We also asked how they rated this supplementary information on a scale of 1 to 10. The final section of the questionnaire used list selection and asked respondents to rate topics from a list from one to ten regarding information they would have liked to receive and how. There were two open ended concluding questions which invited respondents to write free text suggestions on information delivery or general feedback.
This was a blinded observational study, where consultants and Registrars involved in the pre-operative consultation with patients and caregivers (either on a previous occasion or on the day of surgery) were not aware that questionnaires were being distributed specifically to their patients.
Data was entered into a spreadsheet and qualitatively analysed using Microsoft® Excel® Version 12.0 (California, 2008) and Apple Inc. Numbers® Version 3.6.1 (Berkley, 2011). Statistical analysis was performed using a chi-squared test to look at the association between two categorical variables, and a student’s t-test to compare normally distributed data sets. A P value of 0.05 was deemed to be of statistical significance.
Results
Respondent demographics
One hundred and seventy-two questionnaires were returned, 83.1% had been completed by the mother of the child having the procedure. Not all questionnaires were completed in full in each section, thus the number of ‘respondents’ is used to refer to the total number of answers received for each question. Most patients having surgery were in the 2–5 years old age group (49.7%), and 74.9% of parents were aged between 18–40 years. A total of 37.8% had private health insurance. English was the primary language for 81.9%. The highest education level for the respondents was a tertiary degree for 58.1% and high school in 31.7%. Ninety-one point eight percent had attended the doctor’s appointment with their child when the decision was made to proceed with surgery. The majority of patients were there for minor procedures with tonsillectomy, adenoidectomy or grommet insertion being the most common for 95 out of 148 (64.2%). Thirty-three out of 148 (22.3%) respondents were there for an airway procedure and 9 out of 148 (6.1%) for a head and neck major procedure (Table 1).
Table 1
| Characteristics | % |
|---|---|
| Gender | |
| Male | 15.9 |
| Female | 84.1 |
| Age, years | |
| <18 | 1.1 |
| 18–40 | 74.9 |
| 41–65 | 24 |
| >65 | 0 |
| Insurance status | |
| Private | 37.8 |
| Public | 62.2 |
| Language spoken | |
| English | 81.9 |
| NES | 18.1 |
| Highest education level | |
| Primary | 0.6 |
| Secondary | 31.7 |
| Higher degree | 58.1 |
| Other | 9.6 |
| Child’s age, years | |
| 0–2 | 17 |
| 2–5 | 49.7 |
| 6–10 | 22.2 |
| 11–15 | 9.9 |
| >15 | 1.2 |
| Operation | |
| Tonsils/adenoids | 56.8 |
| Airway | 22.3 |
| Grommets | 7.4 |
| Head & neck | 6.1 |
| Nose | 2.7 |
| Other minor | 4.7 |
NES, non English speaking.
The Pre-operative consultation & information given
Pre-operative information in our institution includes consultation through public registrar run clinics, public consultant supervised clinics as well as private consultant rooms. Ninety-four percent of respondents were satisfied with the pre-operative information they received from their doctor. A total of 96.4% recalled a verbal explanation, 37.9% had this information supplemented with a written brochure or pamphlet and only 2 (0.01%) were given a website recommendation.
Parents rated the information provided to them on a scale from 1 to 10 (1 being confusing, untrustworthy and poor quality, 10 being easy to understand, very trustworthy and excellent quality). The information given to them by their doctor was rated a mean of 8.9 out of 10 for ease of understanding, 9.2 out of 10 for trustworthiness and 9 out of 10 for quality. When asked why they were satisfied with the information given to them by their doctor, 60% reflected that they were comfortable with the content and could recall it, however 27.6% said “I trust the team and don’t need to know anymore”. There was poor understanding of the medical hierarchy and many parents (49.7%) indicated they did not know the seniority of who had recommended their child’s surgery (e.g., resident medical officer versus registrar versus consultant surgeon). Out of those attempting to rank the seniority of the team, only 34 out of 89 (38.2%) correctly identified the consultant as the most senior member. Furthermore, only 10 (11.2%) were able to correctly rank the surgical team members.
Patterns of internet use
A total of 96.9% had regular access to the internet with 84.4% admitting to using it multiple times daily. Most respondents (79.4%) used multiple devices to access the internet. This was most commonly a smartphone (89.2%), followed by a computer (80.4%) and lastly a tablet (62%).
Forty-one percent of parents were happy with the information provided from the initial doctor’s consultation and did not research anything further. Table 2 presents the frequency of researchers and non-researchers in various demographic categories. Chi squared tests of independence were performed comparing the two categorical variables of researchers vs. non-researchers with parents gender, age, etc. Our results indicated that parents who had a higher degree researched the internet more than those with only secondary education. This association between education level and researching health information was statistically significant (P=0.0226). Also, statistically significant (P=0.0019) was the association between insurance status and research. Parents or caregivers with private insurance were more likely to have researched than those without insurance. Parents who completely trusted the information given to them by the team and felt that information to be completely understandable were less likely to seek further information from the internet (P=0.0484).
Table 2
| Characteristics | Researched % | Did not research | P value |
|---|---|---|---|
| Gender | |||
| Male | 54.2 | 45.8 | 0.5451 |
| Female | 60.7 | 39.3 | |
| Age | |||
| <40 years | 62.6 | 37.4 | 0.1297 |
| >40 years | 48.7 | 51.4 | |
| Insurance status | |||
| Private | 74.2 | 25.8 | 0.0019* |
| Public | 49.5 | 50.5 | |
| Language spoken | |||
| English | 65.3 | 34.7 | 0.0548 |
| NES | 50 | 50 | |
| Highest education level | |||
| Primary & secondary | 48.5 | 51.5 | 0.0226* |
| Higher degree | 66.7 | 33.3 | |
| Child’s age | |||
| 0–5 years | 63.9 | 36.1 | 0.0944 |
| 6–15 years | 50 | 50 | |
| Operation | |||
| Tonsils/adenoids/grommets | 63.7 | 36.3 | |
| Other minor | 46.7 | 53.3 | 0.1753 |
| Airway | 74.2 | 35.8 | |
| Other major | 46.2 | 53.8 | |
| Pre-operative consultation | |||
| Attended | 59 | 41 | 0.8564 |
| Did not attend | 61.5 | 38.5 | |
| Number of internet access devices | |||
| Only one | 45.2 | 54.8 | 0.0669 |
| More than one | 63.2 | 36.8 | |
| Why they were satisfied with information given | |||
| Understood content | 59 | 41 | 0.0484* |
| Trust the team completely | 39.5 | 60.5 | |
*, statistically significant.
Trends were observed between the categorical variables of parent age, parent gender, child’s age, English speaking background, whether their child was undergoing a major or minor procedure, whether they attended the pre-operative consultation and number of internet access devices they owned, however none of these were statistically significant with regards to whether further information was sought.
Alternative information sourcing
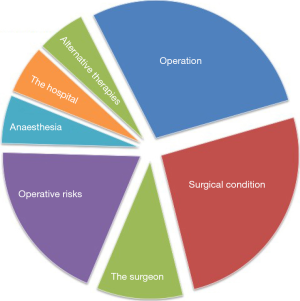
Seventy-three percent admitted to researching the internet, brochures, pamphlets, other health professionals or family and friends. Out of 95 respondents detailing what topics they researched, the operation itself was the most sought-after area (72.6%), followed by their child’s condition (66.3%) and surgical risks (49.5%). Anaesthesia, the hospital itself and alternative treatments were the least commonly researched topics (Figure 1). This additional information impacted decision making in 49.5% of respondents though only 31.8% discussed it with their doctor.
The internet was the most frequently used source of supplementary information for 89% of respondents, and most commonly via popular search engines like Google (73.2%). Only 24.1% and 18.8% of internet users sought more reliable sites such as a known medical website or the hospital/doctors-own website respectively.
Out of non-web based sources, the most commonly accessed were family or friends (27.8%), a general practitioner (27.8%), brochures (19%), a paediatrician (15.1%) and least commonly books (3.2%). Overall, parents felt the best source of information regarding their child’s condition and operation was a verbal explanation from the consultant specialist or team (85.5%). Only 13.8% regarded internet browsing as the best source and no respondents selected the option ‘Blogs, Facebook, online discussion forums, etc.’ as the best source.
Respondents deemed their independent research to be comparably easy to understand, with a mean rating of 8.6 out of 10 though perceived it to be of a lower quality (mean =7.8 out of 10) and to be less trustworthy (mean =7.8 out of 10). There were statistically significant higher ratings for all three aspects of information provided by their doctors than that independently researched, with a P value <0.05 (Table 3), determined using a student’s t-test.
Table 3
| Attributes | Information given | Their research | P value |
|---|---|---|---|
| Easy to understand | 8.9 | 8.6 | 0.0326 |
| Trustworthy | 9.2 | 7.8 | 0.0001 |
| High quality | 9 | 7.8 | 0.0001 |
When asked to compare the content of the information provided and that independently researched, an overwhelming 112 out of 117 (95.7%) described that they were in fact similar. 55 out of 111 said that the information they researched impacted their decision-making, rating it in the range of 6 to 10 on a scale of 1–10 (1 being did not have any impact at all and 10 being very influential). Their mean rating was however different (5.2 out of 10), reflecting it to be mildly influential.
What do parents want?
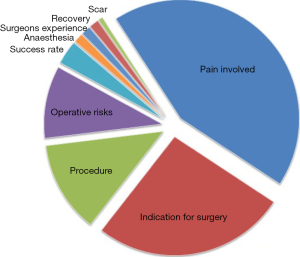
Parents valued a verbal explanation from the surgical team over other information sources (92%), and preferred it to be given at the initial consultation rather than on the day of surgery (75% vs. 18%). Fifty-nine percent wanted information on post-operative care on the day of surgery, 42.7% wanted it prior to discharge, though 34% thought it would have been useful to know at the initial consultation. They ranked most concern about the pain involved with their child’s procedure, followed by the indication for surgery, the operation itself and the risks (Figure 2). Verbal and printed information rather than a website link or download was desirable for communication of these topics, with only 16% preferring to receive a website recommendation.
Discussion
Our study has confirmed that parents and caregivers of children having otolaryngology procedures at our institution source supplementary health information prior to surgery, primarily via the internet. This is not unique to our surgical specialty as the rising use of the internet to inform patients is reflected by research in the local population, national population (4), in a paediatric caregiver population (5,6) and in other western countries (2,7). A more comprehensive review of the literature however, shows that utilisation of the internet for health information sourcing is a heterogeneous phenomenon, finding that rates varied from 11–90% (3). The results presented are in the context of our hospital catchment area including a higher socio-economic group in a large metropolitan setting, as well as a tertiary pattern for referrals. We found that within our population, younger, more educated parents were more likely to have used the internet to research their child’s condition. This association between education (3,5), income, holding private health insurance and younger parents (2,4) has been shown various times to be associated with health seeking behaviours over the internet which may simply reflect ability and accessibility to the information sources.
The idea that patients use the internet to research because they can, and not because the information already provided to them was inadequate is reinforced by the fact that researched information only impacted on decision making in 49.5% of cases; they trusted the information they researched less, rated it to be of a lower quality, and most parents (95.7%) found the information they researched to be similar in content to what their treating team provided. This suggests that their research was for reassurance, curiosity and to reinforce information and management decisions already made. Recent studies have similarly found that though parents research frequently, it rarely has a significant impact (2) or is trusted more than that of a health professional (4,6). Parents used the internet to research general topics and information such as the operation and their child’s condition, which was revealed as the two topics they would like to receive information on through an electronic format. However, they identified specific concerns including post-operative pain and surgical indications as being most important to their understanding. This may be a reflection of the nature of the otolaryngology procedures being undertaken and might have had a different emphasis if a broader surgical population was being surveyed. Parents in our study appeared to use the internet to supplement general medical understanding rather than to clarify specific questions or guide their decision making.
At a local level, we aimed to evaluate the quality of information that we provided to parents and to identify how best to allocate resources to improve this aspect of our surgical service, such as whether to invest time and effort into developing internet based resources. It appears from the feedback that we are doing reasonably well with the pre-operative discussion. This experience was generally positive and our verbal consultations were highly valued by our patients and their parents. Eighty-five point five percent of parents stated that a verbal explanation from the specialist doctor was the best overall source of health information for them. Twenty-five point eight percent of respondents said they “trusted the team and didn’t need to know any more”, reflecting a more traditional, paternalistic doctor-patient relationship. Interestingly, most parents admitted they had absolutely no idea about the hierarchy of our surgical team and could not recall whether the consultant, registrar or resident medical officer had counselled them when their child’s surgery was booked. Greater healthcare transparency is especially important in the public hospital setting where the surgical team members may change from the point of booking a procedure at an outpatient clinic to when the patient presents for surgery. Making sure our staff are wearing name tags, introducing themselves appropriately and explaining the nomenclature of their position including their level of seniority, will help bridge the doctor-patient relationship in this regard.
The supplementary information obtained by parents from their own research was perceived to be slightly less trustworthy and of lower quality than that provided by their doctor, though we did not establish why. The majority of parents (73.2%) used a non-medical non-scientific search engine such as Google, compared to 24.1% interrogating a medical database and 18.8% acquiring information from a health institution website. Even though there are some excellent resources for health education designed for the general public, not all information frequently accessed through popular search engines is reliable, accurate or validated (8). Quantitative studies have found that medical search engines such as MedlinePlus and eMedicine have a large variation in the accuracy of content (49% and 84% respectively), compared to general search engines including Google and Wikipedia, which were accurate less than half of the time (47%) (9).
The internet is the most frequently accessed form of additional information used by parents attending our surgical unit, even though most preferred to be provided with a written brochure/pamphlet describing general information on their child’s condition and planned surgery. The fact that only 31.8% of parents discussed what they researched with their specialist may reflect that it has low impact but may be for other reasons such as not wanting to admit to having needed more information. It also highlights that internet resources are not being discussed in our consultations. Addressing supplementary research, they may have done in the pre-operative period will enhance shared decision making and autonomy.
Recent research supports that the format information is presented to patients in (whether internet or printed pamphlet) is simply a matter of patient preference and does not impact how they value that information (10). When asked this question directly to determine their preference, only 16.4% of our respondents wanted to be recommended a website for pre-operative information. Where other studies have suggested health practitioners should direct parents toward more reliable resources (8), it seems our respondents value the information that comes directly from their doctors more. They sourced general information from the internet but identified that they valued receiving specific information from the surgeons involved in their child’s care on post-operative pain (82.5%) and indications for surgery (50%). The personalised “human aspect” of the doctor-patient relationship thus still underpins our respondent’s health experience.
The aim of our study was to understand the needs of our caregivers and to allocate resources appropriately to improve the quality of our service provision to them. We acknowledge that to truly understand the nature of health-information seeking behaviours and its influence, a prospective survey should have been done at the time of consultation rather than on the day of surgery as there may have been parents who elected for non-surgical treatment depending on their research. Participation in our study was completely voluntary which may have influenced our results. Caregivers were given the questionnaire to complete in their own time while waiting for their child’s operation. The administration clerks distributing the surveys did not monitor the number of questionnaires that were never returned or not completed hence there was no way of performing a demographic analysis of those who did not participate or respond. In addition, the questionnaire was distributed in English only and the respondents would have required a degree of literacy to complete the questions, which also lends our study to some potential biases. The questionnaire format has the advantage of anonymity and is non-obtrusive, however assumed an honest and accurate recollection of the pre-operative consultation, which may have taken place several months prior. There was no way of verifying the reliability of the responses (such as confirming whether the information provided from their doctor was purely verbal or written) which opens up our data to potential inaccuracies. Many of our questions were presented with list style options and there was limited opportunity for free responses. Our questionnaire was not personalised and our findings why people researched did not address disease-specific or patient-specific factors which interview based studies have found to be significant (2,5,7). An interview style of data collection ideally would have helped address more personal reasons however we did not have the resources available for this.
Despite these limitations, the direct feedback obtained from parents in this study has been helpful to reinforce the need for good verbal communication and continued refinement of our doctor-patient relationship. Based on the results of this survey, we have invested in developing written information sheets for our local patient population to supplement the Royal Australasian College of Surgeons brochures detailing common otolaryngology procedures. These sheets specifically provide practical information on the procedure itself and indications, post-operative pain management and tips to improve general recovery, in keeping with the individual treating surgeon’s preferences. Distribution of this information at the time of booking and again by nursing staff at the time of discharge, will hopefully improve our overall quality of care in this aspect of communication. Having the same information available on the hospital website may be of benefit to a smaller group of caregivers. It has the secondary advantage of being a reliable source of health information potentially accessible to those considering a surgical intervention to help guide their decision making.
Conclusions
The internet is the most frequent source of health information accessed by parents attending our surgical unit. Despite this, parents value and trust the pre-operative discussion with their specialist more, compared to the general information they researched on the internet, commonly through non-scientific search engines. This is reassuring for surgeons though reinforces the need for good communication skills and cultivating a good doctor-patient relationship. Information sourcing in our population was not openly used to guide health decision making. The healthcare experience for caregivers at our institution however can be enhanced by providing written information around the time of surgery reiterating specifics about their child’s particular operation, post-operative expectations and pain management.
Acknowledgments
This paper was presented as a poster at the Australian Society of Otolaryngology, Head and Neck Surgery’s Annual Scientific Meeting in Melbourne, 6–8 March 2016.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ajo.2018.01.04). The authors have no conflicts to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was obtained from the Sydney Children’s Hospitals Network Human Research Ethics Committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Australian Bureau of Statistics. Internet Activity, 2015. Canberra: Commonwealth of Australia; updated 6 April 2016; cited 1 July 2016. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/0/00FD2E732C939C06CA257E19000FB410?Opendocument
- Ybarra ML, Suman M. Help seeking behavior and the Internet: a national survey. Int J Med Inform 2006;75:29-41. [Crossref] [PubMed]
- Park E, Kim H, Steinhoff A. Health-Related Internet Use by Informal Caregivers of Children and Adolescents: An Integrative Literature Review. J Med Internet Res 2016;18:e57. [PubMed]
- Australian Child Health Poll. What the public thinks. Sources of child health information: what parents use and trust. Poll 2, March 2016. Parkville, Victoria: The Royal Children’s Hospital Melbourne; updated 2 March 2016; cited 3 April 2016. Available from: https://www.childhealthpoll.org.au/wp-content/uploads/2016/03/ACHP-detailed-report-Poll-2.pdf
- Bianco A, Zucco R, Nobile CG, et al. Parents seeking health-related information on the Internet: cross-sectional study. J Med Internet Res 2013;15:e204. [Crossref] [PubMed]
- Glynn RW, O'Duffy F, O'Dwyer TP, et al. Patterns of Internet and smartphone use by parents of children attending a pediatric otolaryngology service. Int J Pediatr Otorhinolaryngol 2013;77:699-702. [Crossref] [PubMed]
- van der Gugten AC, de Leeuw RJ, Verheij TJ, et al. E-health and health care behaviour of parents of young children: a qualitative study. Scand J Prim Health Care 2016;34:135-42. [Crossref] [PubMed]
- Acar B, Acar M, Ocak E, et al. Accuracy of Internet guidance on pediatric otolaryngology procedures. Int J Pediatr Otorhinolaryngol 2014;78:2190-2. [Crossref] [PubMed]
- Volsky PG, Baldassari CM, Mushti S, et al. Quality of Internet information in pediatric otolaryngology: a comparison of three most referenced websites. Int J Pediatr Otorhinolaryngol 2012;76:1312-6. [Crossref] [PubMed]
- Henney S, Irving R. Prospective, randomised, controlled trial comparing delivery of patient information for functional endoscopic sinus surgery via website versus printed leaflet. J Laryngol Otol 2014;128:249-54; quiz 254. [Crossref] [PubMed]
Cite this article as: Wadhera V, Hwang S, O’Connor L, Soma M. Health information: sourcing patterns and quality improvement prior to surgery. Aust J Otolaryngol 2018;1:4.